US Patent Issued to investigators and students of the University of Puerto Rico



Media Statement
For Immediate Release: Tuesday, November 2, 2021
Contact: Media Relations
(404) 639-3286
Today, CDC Director Rochelle P. Walensky, M.D., M.P.H., endorsed the CDC Advisory Committee on Immunization Practices’ (ACIP) recommendation that children 5 to 11 years old be vaccinated against COVID-19 with the Pfizer-BioNTech pediatric
COVID-19 cases in children can result in hospitalizations, deaths, MIS-C (inflammatory syndromes) and long-term complications, such as “long COVID,” in which symptoms can linger for months. The spread of the Delta variant resulted in a surge of COVID-19 cases in children throughout the summer. During a 6-week period in late June to mid-August, COVID-19 hospitalizations among children and adolescents increased fivefold. Vaccination, along with other preventative measures, can protect children from COVID-19 using the safe and effective vaccines already recommended for use in adolescents and adults in the United States. Similar to what was seen in adult vaccine trials, vaccination was nearly 91 percent effective in preventing COVID-19 among children aged 5-11 years. In clinical trials, vaccine side effects were mild, self-limiting, and similar to those seen in adults and with other vaccines recommended for children. The most common side effect was a sore arm.
COVID-19 vaccines have undergone – and will continue to undergo – the most intensive safety monitoring in U.S. history. Vaccinating children
Distribution of pediatric vaccinations across the country started this week, with plans to scale up to full capacity starting the week of November 8th. Vaccines will be available at thousands of pediatric healthcare provider offices, pharmacies, Federally Qualified Health Centers, and more.
The following is attributable to Dr. Walensky:
“Together, with science leading the charge, we have taken another important step forward in our nation’s fight against the virus that causes COVID-19. We know millions of parents are eager to get their children vaccinated and with this decision, we now have recommended that about 28 million children receive a COVID-19 vaccine. As a mom, I encourage parents with questions to talk to their pediatrician, school nurse or local pharmacist to learn more about the vaccine and the importance of getting their children vaccinated.”
###


From LAB to Community: Portrait of a Symposium

By Eduardo Lamadrid Aguilar, J.D., M.A.C.
Member Community Engagement Coalition Team
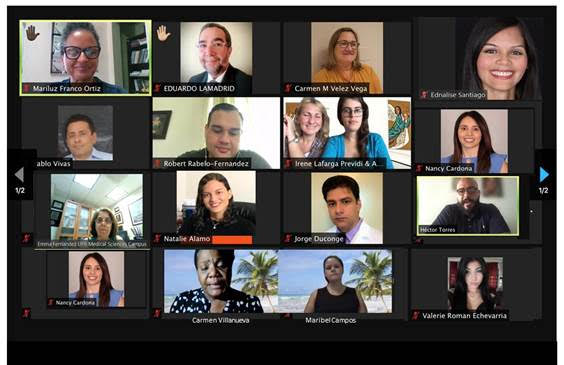
The communities are diverse, as is the research carried out in them. Hence the importance of the recent symposium held by the Community Engagement Core (CEC) of the Center for Collaborative Research on Health Disparities (CCRHD), entitled “From the laboratory to the community: Community engagement efforts in research on health disparities in Puerto Rico”.
This online symposium was held during the mornings of two consecutive days, beginning with a discussion on the main topic of the day, followed by a couple of panels where projects that serve as practical examples of that same topic were presented.
The topic of the first day's discussion was “Community engagement in research projects”, presented by the leaders of the community component, Dr. Carmen Milagros Vélez Vega, Dr. Irene Lafarga Prévidi, and Dr. Ana Cecilia Guzzi Vasques. The first panel consisted of "Experiences of students or research assistants in clinical studies", with the participation of the researchers, Dr. Pablo Vivas and Dr. Jorge Duconge, along with members of their work teams: Ricardo Noriega, Mariela Rivera, and Mariangely Moneró. A second panel on “Community Outreach Efforts” included the participation of Robert Rabelo, and Ednalisse Santiago.
The main theme of the second day was "The return of results to participants", presented by Héctor Torres, who creatively summarized the ways of communicating to the communities those research findings that can positively impact the population’s quality of life.
The first panel "Experiences of students or research assistants in intervention studies" had the participation of the researcher, Dr. Maribel Campos, together with Yari Valle, and Génesis Alvelo. The second panel, corresponding to “Community Outreach Efforts”, also featured contributions from Milane Medina, Nancy Cardona, and an interesting, recorded interview with community leader Carmen Villanueva.
As an interesting fact, each morning session began with breathing exercises for the relaxation and concentration of the participants, and concluded with interactive question and answer sessions, some to underline the importance of the topics discussed, and others to promote a greater sense of belonging among the group of researchers, assistants, and members of the Community Engagement Core.
# # #